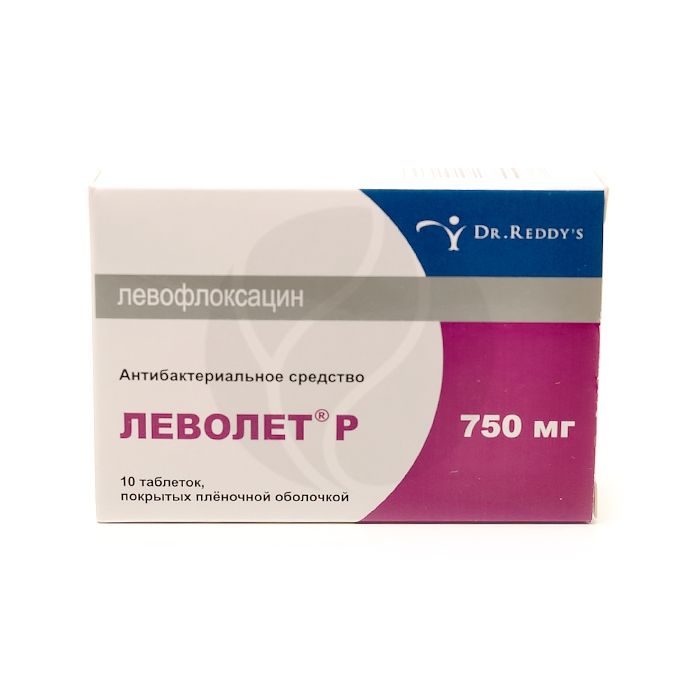
Levolet R tablets 750mg, No. 10
Expiration Date: 05/2027
Russian Pharmacy name:
Леволет Р таблетки 750мг, №10
Infectious and inflammatory diseases caused by pathogens sensitive to levofloxacin:
acute bacterial sinusitis;
community-acquired pneumonia;
complicated urinary tract infections, including pyelonephritis;
complicated infections of the skin and soft tissues.
The drug is taken orally 1 time / day. The tablets should be taken without chewing and with a sufficient amount of liquid (0.5 to 1 cup). The drug can be taken before meals or at any time between meals. The drug should be taken at least 2 hours before or 2 hours after taking antacid drugs containing magnesium and / or aluminum, iron salts or sucralfate. Doses are determined by the nature and severity of the infection, as well as the sensitivity of the suspected pathogen. Do not exceed the recommended dose.
The duration of treatment varies depending on the course of the disease. Considering that the bioavailability of levofloxacin when taken in tablets is 99%, in the case of transferring a patient from IV infusion of LevoletЃ R to taking LevoletЃ R tablets, treatment should be continued at the same dose that was used during IV infusion. Patients with normal renal function or mild renal impairment (CC more than 50 ml / min) Acute bacterial sinusitis: 750 mg 1 time / day; the course of treatment is 5 days.
Community-acquired pneumonia caused by Streptococcus pneumoniae (penicillin-susceptible / moderately susceptible / resistant strains), Haemophilus influenzae (ampicillin-sensitive / resistant strains), Haemophilus parainfluenzae, Mycoplasma pneumoniae, Chlamydia pneumoniae; 750 mg / ml the course of treatment is 5 days.
Complicated urinary tract infections caused by Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, acute pyelonephritis caused by Escherichia coli, including cases of absent bacteremia: 750 mg 1 time / day; the course of treatment is 5 days.
Complicated infections of the skin and soft tissues: 750 mg 1 time / day; the course of treatment is 7-14 days.
Levofloxacin is excreted mainly through the kidneys, therefore, when treating patients with impaired renal function (CC 50-20 ml / min), a dose reduction is required: the recommended dose is 750 mg every 48 hours.
If the liver function is impaired, the dosage regimen does not need to be adjusted, since levofloxacin is metabolized in the liver to an insignificant extent. For elderly patients, no dosage regimen correction is required, except in cases of a decrease in CC to 50 ml / min and below.
Film-coated tablets of white or almost white color, capsule-shaped, biconvex.
1 tab. levofloxacin hemihydrate 768.7 mg,?
which corresponds to the content of levofloxacin 750 mg
Excipients: microcrystalline cellulose (Avicel PH 101) - 76 mg, corn starch - 75.3 mg, colloidal silicon dioxide - 15 mg, crospovidone - 64 mg, hypromellose (15 cps) - 21 mg, microcrystalline cellulose (PH 102) - 90 mg , magnesium stearate - 15 mg.
impaired renal function (with CC less than 20 ml / min due to the impossibility of dosing this dosage form);
epilepsy;
tendon lesions associated with a history of quinolones; pseudoparalytic myasthenia gravis (myasthenia gravis);
children and adolescents up to 18 years of age (due to incomplete growth of the skeleton, since the risk of damage to cartilaginous growth points cannot be completely excluded);
pregnancy;
lactation period (breastfeeding);
hypersensitivity to levofloxacin, other quinolones, as well as any of the auxiliary components of the drug.
With caution: for diseases of the central nervous system, incl. suspicious of the involvement of the central nervous system, predisposing to the occurrence of seizures and lowering the threshold of seizure activity of the brain; in patients who are simultaneously receiving drugs that lower the threshold for seizure readiness of the brain; in patients with a history of psychoses and psychiatric diseases; in patients with latent or manifest deficiency of glucose-6-phosphate dehydrogenase (increased risk of hemolytic reactions during treatment with quinolones); in patients with impaired renal function with CC 20-50 ml / min (mandatory monitoring of renal function is required, as well as correction of the dosage regimen); in the presence of known risk factors for prolongation of the QT interval: in elderly patients; female patients; patients with uncorrected electrolyte disturbances (with hypokalemia,hypomagnesemia); with congenital lengthening of the QT interval; with heart disease (heart failure, myocardial infarction, bradycardia); while taking medications that can lengthen the QT interval; in patients with diabetes mellitus receiving oral hypoglycemic drugs (for example, glibenclamide) or insulin (the risk of hypoglycemia increases); in patients with severe adverse reactions to other fluoroquinolones, for example, severe neurological reactions (increased risk of similar adverse reactions when using levofloxacin).in patients with diabetes mellitus receiving oral hypoglycemic drugs (for example, glibenclamide) or insulin (the risk of hypoglycemia increases); in patients with severe adverse reactions to other fluoroquinolones, for example, severe neurological reactions (increased risk of similar adverse reactions when using levofloxacin).in patients with diabetes mellitus receiving oral hypoglycemic drugs (for example, glibenclamide) or insulin (the risk of hypoglycemia increases); in patients with severe adverse reactions to other fluoroquinolones, for example, severe neurological reactions (increased risk of similar adverse reactions when using levofloxacin).
pharmachologic effect
An antibacterial drug of the group of fluoroquinolones with a broad spectrum of action. Blocks DNA gyrase (topoisomerase II) and topoisomerase IV, disrupts supercoiling and stitching of DNA breaks, inhibits DNA synthesis, and causes deep morphological changes in the cytoplasm, cell wall and membranes.
Levofloxacin is active against the following strains of microorganisms, both in vitro and in vivo.
Sensitive microorganisms (MIC ? 2 mg / ml)
Aerobic gram-positive microorganisms: Bacillus anthracis, Corynebacterium diphtheriae, Corynebacterium jeikeium, Enterococcus spp. (including Enterococcus faecalis), Listeria monocytogenes, Staphylococcus spp. (coagulase-negative methicillin-susceptible / moderately susceptible strains, leukotoxin-containing strains), including Staphylococcus aureus (methicillin-susceptible strains), Staphylococcus epidermidis (methicillin-susceptible strains); Streptococcus spp. groups C and G, Streptococcus agalactiae, Streptococcus pneumoniae (penicillin-sensitive / moderately sensitive / resistant strains), Streptococcus pyogenes, Streptococcus viridans (penicillin-sensitive / resistant strains).
Aerobic gram-negative microorganisms: Acinetobacter spp. (including Acinetobacter baumannil), Actinobacillus actinomycetemcomitans, Citrobacter freundii, Eikenella corrodens, Enterobacter spp. (including Enterobacter cloacae, Enterobacter aerogenes), Escherichia coli, Gardnerella vaginalis, Haemophilus ducreyi, Haemophilus influenzae (ampicillin-sensitive / resistant strains), Haemophilus parainfluenzae, Helicobacter pylori s, Klebs. (including Klebsiella oxytoca, Klebsiella pneumoniae), Moraxella catarrhalis (strains producing and non-producing ?-lactamase), Morganella morganii, Neisseria gonorrhoeae (producing and non-producing strains. (including Pasteurella conis, Pasteurella dagmatis, Pasteurella multocida), Proteus mirabilis, Proteus vulgaris, Providencia spp. (incl.Providencia rettgeri, Providencia stuartii), Pseudomonas spp. (including Pseudomonas aeruginosa), Serratia spp. (including Serratia marcescens), Salmonella spp.
Anaerobic microorganisms: Bacteroides fragilis, Bifidobacterium spp., Clostridium perfringens, Fusobacterium spp., Peptostreptococcus spp., Propionibacterium spp., Veilonella spp.
Other microorganisms: Bartonella spp., Chlamydia pneumoniae, Chlamydia psittaci, Chlamydia trachomatis, Legionella pneumophila, Legionella spp., Mycobacterium spp. (including Mycobacterium leprae, Mycobacterium tuberculosis), Mycoplasma hominis, Mycoplasma pneumoniae, Rickettsia spp., Ureaplasma urealyticum.
Moderately sensitive microorganisms (MIC ? 4 mg / l)
Aerobic gram-positive microorganisms: Corynebacterium urealyticum, Corynebacterium xerosis, Enterococcus faecium, Staphylococcus epidermidis (methicillin-resistant strains), Staphylococcus haemolyticus (methicillin-resistant strains).
Aerobic gram-negative microorganisms: Campylobacter jejuni, Campylobacter coli.
Anaerobic microorganisms: Prevotella spp., Porphyromonas spp.
Resistant microorganisms (MIC ? 8 mg / l)
Aerobic gram-positive microorganisms: Staphylococcus aureus (methicillin-resistant strains), other Staphylococcus spp. (coagulase-negative methicillin-resistant strains).
Aerobic gram-negative microorganisms: Alcaligenes xylosoxidans.
Anaerobic microorganisms: Bacteroides thetaiotaomicron.
Other microorganisms: Mycobacterium avium.
Resistance
Resistance to levofloxacin develops as a result of a stepwise process of mutation of genes encoding both type II topoisomerases: DNA gyrase and topoisomerase IV. Other mechanisms of resistance, such as the mechanism of influence on the penetration barriers of the microbial cell (characteristic of Pseudomonas aeruginosa) and the efflux mechanism, can also reduce the sensitivity of the microorganism to levofloxacin.
Due to the peculiarities of the mechanism of action of levofloxacin, there is usually no cross-resistance between levofloxacin and other antimicrobial agents.
Clinical efficacy (efficacy in clinical trials in the treatment of infections caused by the microorganisms listed below):
aerobic gram-positive microorganisms: Enterococcus faecalis, Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes;
aerobic gram-negative microorganisms: Citrobacter freundii, Enterobacter cloacae, Escherichia coli, Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Moraxella (Branhamella) catarrhalis, Morganella morganii, Proteus mirabilis, Pseudomonasse
others: Chlamydia pneumoniae, Legionella pneumophila, Mycoplasma pneumoniae.
Pharmacokinetics
Suction
After taking the drug inside, it is quickly and almost completely absorbed from the gastrointestinal tract. Food intake has little effect on the rate and completeness of absorption. Bioavailability - 99%. TCmax - 1-2 hours; when taken at a dose of 750 mg, the average Cmax is 8 ?g / ml.
Distribution
Plasma protein binding - 30-40%.
It penetrates well into organs and tissues: lungs, bronchial mucosa, phlegm, organs of the genitourinary system, polymorphonuclear leukocytes, alveolar macrophages.
Metabolism
In the liver, a small part of levofloxacin is oxidized and / or deacetylated.
Withdrawal
T1 / 2 is 6-8 hours. After a single oral dose of 750 mg T1 / 2 - 7.5 ± 0.9 hours. It is excreted mainly by the kidneys by glomerular filtration and tubular secretion. Renal clearance is 70% of the total clearance. Less than 5% of levofloxacin is excreted as metabolites. In the urine for a period of 24 hours, 70% is found unchanged, and for 48 hours - 87% taken orally. In feces for a period of 72 hours, 4% of the dose taken orally is detected.
Pharmacokinetics in special patient groups
In renal failure, a decrease in drug clearance and its excretion by the kidneys depends on the degree of CC decrease. Levofloxacin is not excreted from the body by hemodialysis or continuous ambulatory peritoneal dialysis.
Side effect
The following side effects are presented in accordance with the following gradation of frequency of their occurrence: very often (> 1/10); often (1 / 10-1 / 100); infrequently (1 / 100-1 / 1000); rarely (1/1000, <1/10 000); very rare (<1/10 000); the frequency is unknown (according to the available data, it is not possible to determine the frequency of occurrence).
From the side of the cardiovascular system: rarely - sinus tachycardia, palpitations, decreased blood pressure; frequency unknown (post-marketing data) - prolongation of the QT interval, ventricular arrhythmias, ventricular tachycardia, ventricular tachycardia of the 'pirouette' type, which can lead to cardiac arrest.
From the hematopoietic system: infrequently - leukopenia, eosinophilia; rarely - neutropenia, thrombocytopenia; frequency is unknown (post-marketing data) - pancytopenia, agranulocytosis, hemolytic anemia.
From the nervous system: often - headache, dizziness; infrequently - drowsiness, tremors, dysgeusia; rarely - paresthesia, convulsions; frequency unknown (post-marketing data) - peripheral sensory neuropathy, peripheral sensory-motor neuropathy, dyskinesia, extrapyramidal disorders, ageusia, parosmia, including loss of smell; fainting, benign intracranial hypertension.
Mental disorders: often - insomnia; infrequently - a feeling of anxiety, anxiety, confusion; rarely - mental disorders (for example, hallucinations, paranoia), depression, agitation, sleep disturbances, nightmares; frequency unknown (post-marketing data) - self-harming behavior disorders, including suicidal thoughts and suicidal attempts.
From the side of the organ of vision: very rarely - visual impairments, such as blurring of the visible image; frequency unknown - transient loss of vision, uveitis.
From the side of the organ of hearing and labyrinth disorders: infrequently - vertigo; rarely - ringing in the ears; frequency unknown (post-marketing data) - hearing loss, hearing loss.
From the respiratory system: infrequently - shortness of breath; frequency unknown (post-marketing data) - bronchospasm, allergic pneumonitis.
From the digestive system: often - diarrhea, vomiting, nausea, increased activity of liver enzymes in the blood (for example, ALT, AST), increased ALP and GGT activity; infrequently - anorexia, abdominal pain, dyspepsia, flatulence, constipation, increased concentration of bilirubin in the blood; frequency unknown (post-marketing data) - stomatitis, hemorrhagic diarrhea, which in very rare cases can be a sign of enterocolitis, including pseudomembranous colitis, pancreatitis, severe liver failure, including cases of acute liver failure, sometimes with a fatal outcome, especially in patients with severe underlying disease (for example, in patients with sepsis), hepatitis, jaundice.
From the urinary system: infrequently - an increase in the concentration of creatinine in the blood serum; rarely - acute renal failure (for example, due to the development of interstitial nephritis).
Skin and subcutaneous tissue disorders: infrequently - rash, itching, urticaria, hyperhidrosis; frequency unknown (post-marketing data) - toxic epidermal necrolysis, Stevens-Johnson syndrome, exudative erythema multiforme, photosensitivity reactions, leukocytoclastic vasculitis. Reactions from the skin and mucous membranes can sometimes develop even after taking the first dose of the drug.
From the musculoskeletal system: infrequently - arthralgia, myalgia; rarely - tendon involvement, including tendonitis (eg, Achilles tendon), muscle weakness, which can be especially dangerous in patients with pseudoparalytic myasthenia gravis (myasthenia gravis); the frequency is unknown (post-marketing data) - rhabdomyolysis, tendon rupture (for example, Achilles tendon) - this side effect can be observed within 48 hours after the start of treatment and can be bilateral; ligament rupture, muscle tear, arthritis.
From the side of metabolism: rarely - hypoglycemia, especially in patients with diabetes mellitus (possible signs of hypoglycemia: 'wolfish' appetite, nervousness, perspiration, tremors); frequency unknown - hyperglycemia, hypoglycemic coma.
Infectious and parasitic diseases: infrequently - fungal infections, development of resistance of pathogenic microorganisms.
From the immune system: rarely - angioedema; frequency is unknown (post-marketing data) - anaphylactic shock, anaphylactoid shock. Anaphylactic and anaphylactoid reactions can sometimes develop even after taking the first dose of the drug.
Others: infrequently - asthenia; rarely - pyrexia; frequency unknown - pain (including pain in the back, chest, limbs).
Other Potential Undesirable Effects Relating to All Fluoroquinolones
From the side of metabolism: very rarely - attacks of porphyria in patients already suffering from this disease.
Application during pregnancy and lactation
Levofloxacin is contraindicated during pregnancy and lactation.
Application for violations of liver function
If the liver function is impaired, the dosage regimen does not need to be adjusted, since levofloxacin is metabolized in the liver to an insignificant extent.
Application for impaired renal function
When treating patients with impaired renal function (CC 50-20 ml / min), a decrease in the dose of the drug is required.
Application in children
Contraindicated: children and adolescents under 18 years of age.
Use in elderly patients
For elderly patients, no dosage adjustment is required, except in cases of a decrease in CC to 50 ml / min and below.
special instructions
As with the use of other antimicrobial agents, it is recommended to continue treatment with LevoletЃ R for at least 48-72 hours after normalization of body temperature or after reliable eradication of the pathogen.
The prevalence of acquired resistance in cultured strains of microorganisms can vary depending on the geographic region and over time. For the treatment of severe infections or in case of ineffectiveness of treatment, a microbiological diagnosis should be established with the isolation of the pathogen and determination of its sensitivity to levofloxacin.
Methicillin-resistant Staphylococcus aureus is highly likely to be resistant to fluoroquinolones, including lsvofloxacin. Therefore, lsvofloxacin is not recommended for the treatment of established or suspected infections caused by methicillin-resistant Staphylococcus aureus, unless laboratory tests have confirmed the susceptibility of this organism to levofloxacin. When treating elderly patients, it should be borne in mind that renal dysfunction is characteristic of patients of this age group.
In severe cases of Streptococcus pneumoniae pneumonia, levofloxacin may not provide an optimal therapeutic effect. During treatment with LevoletЃ R, a seizure attack may develop in patients with previous brain damage caused, for example, by a stroke or severe traumatic brain injury.
Although photosensitization with the use of levofloxacin develops very rarely, to prevent its development, patients are not recommended during treatment and within 48 hours after the end of treatment with levofloxacin to be exposed without special need to intense solar or artificial ultraviolet radiation (for example, to visit a solarium).
If pseudomembranous colitis is suspected, levofloxacin should be discontinued immediately and appropriate treatment should be initiated. In such cases, drugs that inhibit intestinal motility cannot be used.
–едко наблюдаемый при применении левофлоксацина тендинит (прежде всего, воспаление ахиллова сухожили¤) может приводить к разрыву сухожилий. Ётот побочный эффект может развитьс¤ в течение 48 ч после начала лечени¤ и может быть двусторонним. ѕациенты пожилого возраста более склонны к тендиниту. ѕри одновременном применении v — повышаетс¤ риск разрыва сухожилий. ѕри подозрении на тендинит следует немедленно прекратить лечение препаратом ЋеволетЃ – и начать соответствующее лечение пораженного сухожили¤.
Ћевофлоксацин может вызывать серьезные, потенциально фатальные, реакции гиперчувствительности (ангионевротический отек, анафилактический шок) даже при применении в начальных дозах. ѕациентам следует немедленно прекратить прием препарата и обратитьс¤ к врачу.
ѕри приеме левофлоксацина наблюдались случаи т¤желых буллезных кожных реакций, таких как синдром —тивенса-?жонсона или токсический эпидермальный некролиз. ¬ случае развити¤ каких-либо реакций со стороны кожи или слизистых оболочек пациент должен немедленно обратитьс¤ к врачу и не продолжать лечени¤ до его консультации.
—ообщалось о случа¤х развити¤ печеночного некроза, включа¤ развитие фатальной печеночной недостаточности при применении левофлоксацина, главным образом, у пациентов с т¤желыми основными заболевани¤ми, например, с сепсисом. ѕациенты должны быть предупреждены о необходимости прекращени¤ лечени¤ и срочного обращени¤ к врачу в случае по¤влени¤ признаков и симптомов поражени¤ печени, таких как анорекси¤, желтуха, потемнение мочи, зуд и боли в животе.
ѕациенты с дефицитом глюкозо-6-фосфатдегидрогеназы имеют предрасположенность к гемолитическим реакци¤м (гемолиз) при лечении хинолонами. ¬ св¤зи с этим лечение таких пациентов левофлоксацином следует проводить с осторожностью.
“.к. левофлоксацин экскретируетс¤ главным образом с мочой, у пациентов с почечной недостаточностью требуетс¤ об¤зательный контроль функции почек.
Ћюба¤ терапи¤ противомикробными средствами может вызывать изменени¤ микрофлоры, котора¤ в норме присутствует у человека. ѕо этой причине может произойти усиленное размножение бактерий и грибов, устойчивых к примен¤емому противомикробному препарату (вторична¤ инфекци¤, суперинфекци¤), которое в редких случа¤х может потребовать дополнительного лечени¤.
¬озможно удлинение интервала QT у пациентов, получавших фторхинолоны, включа¤ левофлоксацин. ѕри применении левофлоксацина следует соблюдать осторожность у пациентов с известными факторами риска удлинени¤ интервала QT: пожилой возраст; нарушение электролитного баланса (гипокалиеми¤, гипомагниеми¤); синдром врожденного удлинени¤ интервала QT; заболевани¤ сердца (сердечна¤ недостаточность, инфаркт миокарда, брадикарди¤); одновременный прием лекарственных средств, способных удлин¤ть интервал QT.
” пациентов с сахарным диабетом, получающих гипогликемические средства дл¤ приема внутрь (например, глибенкламид) или инсулин, при применении левофлоксацина возрастает риск развити¤ гипогликемии. “аким пациентам требуетс¤ мониторинг концентрации глюкозы в крови.
” пациентов, получающих фторхинолоны, включа¤ левофлоксацин, отмечалась сенсорна¤ и сенсорно-моторна¤ периферическа¤ невропати¤, начало которой может быть быстрым. ѕри по¤влении у пациента симптомов невропатии применение левофлоксацина следует прекратить дл¤ снижени¤ возможного риска развити¤ необратимых изменений. ‘торхинолоны, включа¤ левофлоксацин, могут усиливать мышечную слабость и вызывать обострение псевдопаралитической миастении. ѕрименение левофлоксацина у пациентов с установленным диагнозом псевдопаралитической миастении не рекомендуетс¤.
ѕсихотические реакции при применении хинолонов, включа¤ левофлоксацин, в очень редких случа¤х прогрессировали до развити¤ суицидальных мыслей и нарушений поведени¤ с причинением себе вреда (иногда после приема разовой дозы). ѕри развитии таких реакций лечение левофлоксацином следует прекратить и назначить соответствующую терапию. —ледует с осторожностью назначать препарат пациентам с психозами или пациентам, имеющим в анамнезе психические заболевани¤.
ѕри развитии любых нарушений зрени¤, в т.ч. нечеткости зрени¤, необходима немедленна¤ консультаци¤ офтальмолога.
” пациентов, принимающих левофлоксацин, определение опиатов в моче может приводить к ложноположительным результатам, которые следует подтверждать более специфическими методами.
Ћевофлоксацин может ингибировать рост Mycobacterium tuberculosis и приводить в дальнейшем к ложноотрицательным результатам бактериологического диагноза туберкулеза.
¬ли¤ние на способность к вождению автотранспорта и управлению механизмами
¬ период лечени¤ левофлоксацином следует воздержатьс¤ от управлени¤ транспортными средствами и выполнени¤ других потенциально опасных видов де¤тельности, требующих повышенной концентрации внимани¤ и быстроты психомоторных реакций, поскольку возможно развитие головокружени¤, сонливости и расстройства зрени¤.
ѕередозировка
—имптомы: спутанность сознани¤, головокружение, нарушени¤ сознани¤, судороги по типу эпилептических припадков, тошнота, эрозивные поражени¤ слизистой оболочки ? “, удлинение интервала QT, галлюцинации, тремор.
Ћечение: симптоматическое, диализ (гемодиализ, перитонеальный диализ, посто¤нный перитонеальный диализ) неэффективен. —пецифического антидота не существует. “ребуетс¤ мониторинг Ё v. ¬ случае острой передозировки показано промывание желудка и введение антацидов дл¤ защиты слизистой оболочки желудка.
Ћекарственное взаимодействие
Ћевофлоксацин увеличивает “1/2 циклоспорина.
ѕолноту всасывани¤ левофлоксацина снижают лекарственные средства, угнетающие моторику кишечника: сукральфат, антацидные лекарственные средства, содержащие соли алюмини¤ и магни¤, диданозин (только лекарственные формы, содержащие в качестве буфера алюминий или магний), а также препараты, содержащие соли железа. —оли кальци¤ оказывают минимальный эффект на абсорбцию левофлоксацина при его приеме внутрь. Ћевофлоксацин следует принимать не менее чем за 2 ч до или через 2 ч после приема этих средств.
Ќѕ¬— (фенбуфен) и теофиллин при одновременном применении с фторхинолонами снижают порог судорожной готовности головного мозга.
?иметидин и лекарственные средства, блокирующие канальцевую секрецию, замедл¤ют выведение левофлоксацина.
ѕри одновременном применении с непр¤мыми антикоагул¤нтами, производными кумарина необходим контроль ћЌќ.
¬озможно удлинение интервала QT при одновременном применении левофлоксацина со следующими препаратами:
антиаритмические IA (хинидин, прокаинамид, гидрохиниднн, дизопирамид и другие) и III (амиодарон, соталол, дофетидил, ибутилид и другие) классов;
трициклические антидепрессанты;
нейролептики (фенотиазин, пимозид, сертиндол, галоперидол, сультоприд и другие);
противомикробные препараты (спарфлоксацин, антибиотики группы макролидов; пентамидин, галофантрин и другие противомал¤рийные препараты);
антигистаминные препараты (астемизол, терфенадин, мизоластин, эбастин);
другие (цизаприд, винкамин в/в, бепридил, дифемапил).
ѕри одновременном применении с v — возрастает риск развити¤ тендинита и разрыва сухожилий.
vипогликемические препараты увеличивают веро¤тность гипер- и гипогликемии, поэтому необходим строгий мониторинг концентрации глюкозы в крови.
Clinical and pharmacological studies carried out to study the possible pharmacokinetic interactions of levofloxacin with digoxin, glibenclamide, ranitidine and warfarin showed that the pharmacokinstics of levofloxacin when used simultaneously with these drugs does not change sufficiently to be of clinical significance.