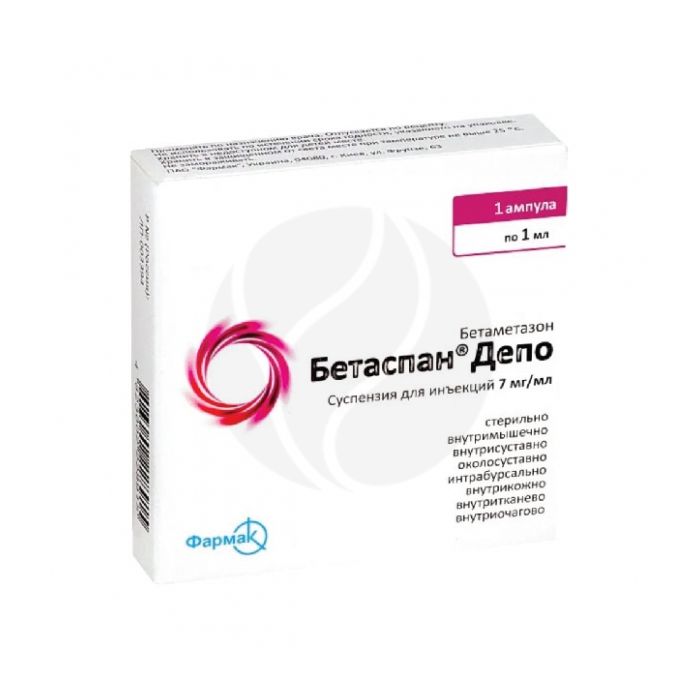
Betaspan Depo suspension for injection 7mg / ml, 1ml No. 1
Russian Pharmacy name:
Бетаспан Депо суспензия д/инъекций 7мг/мл, 1мл №1
Treatment in adult conditions and diseases in which GCS therapy allows to achieve the desired clinical effect (it should be borne in mind that for some diseases GCS therapy is additional and does not replace standard therapy):
diseases of the musculoskeletal system and soft tissues, incl. rheumatoid arthritis, osteoarthritis, bursitis, ankylosing spondylitis, epicondylitis, coccygodynia, torticollis, ganglion cyst, fasciitis;
allergic diseases, incl. bronchial asthma, hay fever (pollinosis), allergic bronchitis, seasonal or perennial rhinitis, drug allergies, serum sickness, insect bite reactions;
dermatological diseases, incl. atopic dermatitis, coin-like eczema, neurodermatitis, contact dermatitis, severe photodermatitis, urticaria, lichen planus, alopecia areata, discoid lupus erythematosus, psoriasis, keloid scars, pemphigus vulgaris, cystic acne;
systemic connective tissue diseases, including systemic lupus erythematosus, scleroderma, dermatomyositis, periarteritis nodosa;
hemoblastosis (palliative therapy of leukemia and lymphomas in adults; acute leukemia in children);
primary or secondary insufficiency of the adrenal cortex (with the obligatory simultaneous use of mineralocorticosteroids).
Other diseases and pathological conditions requiring systemic corticosteroids therapy (adrenogenital syndrome, regional ileitis, pathological changes in the blood, if the use of corticosteroids is necessary).
In / m, intraarticular, periarticular, intrabursal, intravenous, interstitial and intrafocal injection.
The small size of the crystals of betamethasone dipropionate makes it possible to use needles of small diameter (up to 26 gauge) for intravenous injection and injection directly into the lesion.
You can not enter in / in and s / c.
Strict adherence to the rules of asepsis is mandatory when using the drug.
Shake the syringe before administering the drug.
The dosage regimen and the route of administration are set individually, depending on the indications, the severity of the disease and the patient's response.
In case of systemic therapy, the initial dose of BetaspanЃ Depo in most cases is 1Ц2 ml. The introduction is repeated as needed, depending on the patient's condition.
IM introduction
The intramuscular injection of BetaspanЃ Depo should be carried out deep into the muscle, while selecting large muscles and avoiding contact with other tissues (to prevent tissue atrophy).
In severe conditions requiring emergency measures, the initial dose is 2 ml of the drug.
For various dermatological diseases, as a rule, it is sufficient to administer 1 ml of the drug.
In diseases of the respiratory system, the onset of action of the drug occurs within a few hours after the i / m injection.
With bronchial asthma, hay fever, allergic bronchitis and allergic rhinitis, a significant improvement in the condition is achieved after the introduction of 1-2 ml of the drug.
In acute and chronic bursitis, the initial dose for intramuscular injection is 1Ц2 ml of the drug. Several repeated injections are performed if necessary.
If a satisfactory clinical response does not occur after a certain period of time, the drug should be discontinued and another therapy should be prescribed.
Local introduction
With local administration, the simultaneous use of a local anesthetic drug is necessary only in rare cases. If it is desired, then use 1 or 2% solutions of procaine hydrochloride or lidocaine, which do not contain methylparaben, propylparaben, phenol and other similar substances. In this case, mixing is carried out in a syringe, first drawing the required dose of BetaspanЃ Depot into the syringe from the vial. Then, the required amount of local anesthetic is taken from the ampoule into the same syringe and shaken for a short period of time.
In acute bursitis (subdeltoid, subscapularis, ulnar and pre-patellar), injecting 1-2 ml of the drug into the synovial bursa relieves pain and restores joint mobility within a few hours. After the relief of exacerbation in chronic bursitis, smaller doses of the drug are used.
In acute tenosynovitis, tendinitis and peritendinitis, one injection of the drug improves the patient's condition; in chronic cases, the injection is repeated depending on the patient's response. Avoid injecting the drug directly into the tendon.
Intra-articular administration of the drug in a dose of 0.5Ц2 ml relieves pain, limitation of joint mobility in rheumatoid arthritis and osteoarthritis within 2Ц4 hours after administration. The duration of the therapeutic effect varies considerably and can be 4 or more weeks.
The recommended doses of the drug when injected into large joints are from 1 to 2 ml; in the middle - 0.5-1 ml; small - 0.25-0.5 ml.
In some dermatological diseases, intravenous administration of the drug directly into the lesion is effective, the dose is 0.2 ml / cm2. The lesion is evenly injected using a tuberculin syringe and a needle with a diameter of about 0.9 mm. The total amount of the injected drug in all areas should not exceed 1 ml for 1 week. For injection into the lesion, it is recommended to use a tuberculin syringe with a 26-gauge needle.
Recommended single doses of the drug (with an interval between injections of 1 week) for bursitis: with callousness - 0.25-0.5 ml (as a rule, 2 injections are effective), with a spur - 0.5 ml, with limited mobility of the big toe - 0.5 ml, with synovial cyst - 0.25Ц0.5 ml, with tendosynovitis - 0.5 ml, with acute gouty arthritis - 0.5Ц1 ml. A tuberculin syringe with a 25-gauge needle is suitable for most injections.
After the therapeutic effect is achieved, the maintenance dose is selected by gradually reducing the dose of BetaspanЃ Depo administered at appropriate intervals. The decrease is continued until the minimum effective dose is reached.
If a stressful situation arises or is threatened (not related to the disease), it may be necessary to increase the dose of the drug. Cancellation of the drug after prolonged therapy is carried out by gradually reducing the dose. The patient's condition is monitored for at least a year after the end of long-term therapy or use in high doses.
Suspension for injection is transparent, colorless or yellowish in color, slightly viscous, containing easily suspended particles of white or almost white color; when agitated, a suspension of white or almost white color is formed.
1 ml betamethasone dipropionate 6.43 mg,
which corresponds to the content of betamethasone 5 mg
betamethasone sodium phosphate 2.63 mg,
which corresponds to the content of betamethasone 2 mg
Excipients: methyl parahydroxybenzoate (E218) - 1.3 mg, propyl parahydroxybenzoate (E216) - 0.2 mg, benzyl alcohol - 9 mg, sodium chloride - 5.5 mg, sodium hydrogen phosphate - 0.6 mg, disodium edetate dihydrate - 0.1 mg, sodium carmellose - 5.2 mg, polysorbate 80 - 0.5 mg, macrogol 4000 - 25 mg, water d / i - up to 1 ml.
With short-term use for health reasons, the only contraindication is
hypersensitivity;
IV, SC, epidural, intrathecal administration;
injection directly into the tendons of the muscles;
disorders of coagulation (including treatment with anticoagulants), cerebral edema due to traumatic brain injury;
the period of breastfeeding, the simultaneous administration of immunosuppressive doses with live and attenuated vaccines;
For intra-articular administration:previous arthroplasty, pathological bleeding (endogenous or caused by the use of anticoagulants), intra-articular bone fracture, infectious (septic) inflammatory process in the joint and periarticular infections (including history), as well as a general infectious disease, pronounced periarticular osteoporosis, no signs inflammation in the joint ('dry' joint, for example, in osteoarthritis without synovitis), pronounced bone destruction and deformation of the joint (sharp narrowing of the joint space, ankylosis), joint instability as an outcome of arthritis, aseptic necrosis of the epiphyses of the bones forming the joint; introduction into the intervertebral space.
Carefully
Parasitic and infectious diseases of a viral, fungal or bacterial nature (currently or recently transferred, including recent contact with a patient) - herpes simplex, herpes zoster (viremic phase), chickenpox, measles; amebiasis, strongyloidosis (established or suspected); systemic mycosis; active and latent tuberculosis. Application for severe infectious diseases is permissible only against the background of specific therapy.
Post-vaccination period (a period lasting 8 weeks before and 2 weeks after vaccination), lymphadenitis after BCG vaccination. Immunodeficiency states (including AIDS or HIV infection).
Diseases of the gastrointestinal tract: gastric ulcer and duodenal ulcer, esophagitis, gastritis, acute or latent peptic ulcer, recently created intestinal anastomosis, ulcerative colitis with the threat of perforation or abscess formation, diverticulitis.
Diseases of the cardiovascular system: recent myocardial infarction (in patients with acute and subacute myocardial infarction, the necrosis focus may spread, the formation of scar tissue slows down and, as a result, rupture of the heart muscle), decompensated chronic heart failure, arterial hypertension, hyperlipidemia).
Endocrine diseases: diabetes mellitus (including impaired carbohydrate tolerance), thyrotoxicosis, hypothyroidism, Itsenko-Cushing's disease.
Severe chronic renal and / or hepatic failure, nephrourolithiasis.
Hypoalbuminemia and conditions predisposing to its occurrence.
Systemic osteoporosis, myasthenia gravis, acute psychosis, obesity (III-IV grade), poliomyelitis (except for the form of bulbar encephalitis), open and closed angle glaucoma, pregnancy, lactation.
For intra-articular administration: general serious condition of the patient, ineffectiveness (or short duration) of the action of 2 previous injections (taking into account the individual properties of the GCS used).
pharmachologic effect
GKS. It has anti-inflammatory, anti-allergic, desensitizing, anti-shock, anti-toxic and immunosuppressive effects, and also has a pronounced and varied effect on various types of metabolism.
Suppresses the release of ACTH and beta-lipotropin by the pituitary gland, but does not reduce the level of circulating beta-endorphin. Inhibits the secretion of TSH and FSH.
Increases the excitability of the central nervous system, reduces the number of lymphocytes and eosinophils, increases the number of erythrocytes (stimulates the production of erythropoietins).
Interacts with specific cytoplasmic receptors and forms a complex that penetrates the cell nucleus and stimulates the synthesis of mRNA; the latter induces the formation of proteins, incl. lipocortin mediating cellular effects. Lipocortin inhibits phospholipase A2, inhibits the release of arachidonic acid and inhibits the synthesis of endoperoxides, prostaglandins, leukotrienes, which promote inflammation and allergies.
The anti-inflammatory effect is associated with inhibition of the release of inflammatory mediators by eosinophils; inducing the formation of lipocortin and reducing the number of mast cells that produce hyaluronic acid; with a decrease in capillary permeability; stabilization of cell membranes and membranes of organelles (especially lysosomal).
Antiallergic effect develops as a result of suppression of the synthesis and secretion of allergy mediators, inhibition of the release from sensitized mast cells and basophils of histamine and other biologically active substances, T- and B-lymphocytes, mast cells, a decrease in the sensitivity of effector cells to allergy mediators, inhibition of antibody production, changes in immune the response of the body.
The anti-shock and antitoxic effect is associated with an increase in blood pressure (due to an increase in the concentration of circulating catecholamines and restoration of the sensitivity of adrenergic receptors to them, as well as vasoconstriction), a decrease in the permeability of the vascular wall, membrane-protective properties, activation of liver enzymes involved in the metabolism of endo- and xenobiotics.
In COPD, the action is mainly based on inhibition of inflammatory processes, inhibition of the development or prevention of edema of the mucous membranes, inhibition of eosinophilic infiltration of the submucous layer of the bronchial epithelium, deposition of circulating immune complexes in the mucous membrane of the bronchi, as well as inhibition of erosion and desquamation of the mucous membrane. Increases the sensitivity of beta-adrenergic receptors of the bronchi of small and medium caliber to endogenous catecholamines and exogenous sympathomimetics, reduces the viscosity of mucus by inhibiting or reducing its production.
The immunosuppressive effect is due to inhibition of the release of cytokines (interleukin-1, interleukin-2, interferon gamma) from lymphocytes and macrophages.
Suppresses the synthesis and secretion of ACTH and, secondarily, the synthesis of endogenous GCS. It inhibits connective tissue reactions during the inflammatory process and reduces the possibility of scar tissue formation.
Protein metabolism: reduces the amount of protein in the plasma (due to globulins) with an increase in the albumin / globulin ratio, increases the synthesis of albumin in the liver and kidneys; enhances protein catabolism in muscle tissue.
Lipid metabolism: increases the synthesis of higher fatty acids and TG, redistributes fat (fat accumulation mainly in the shoulder girdle, face, abdomen), leads to the development of hypercholesterolemia.
Carbohydrate metabolism: increases the absorption of carbohydrates from the gastrointestinal tract; increases the activity of glucose-6-phosphatase, leading to an increase in the flow of glucose from the liver into the blood; increases the activity of phosphoenolpyruvate carboxylase and the synthesis of aminotransferases, leading to the activation of gluconeogenesis.
Water-electrolyte metabolism: retains sodium and water in the body, stimulates the excretion of potassium, reduces the absorption of calcium from the gastrointestinal tract, 'flushes' calcium from the bones, and increases excretion by the kidneys.
Betamethasone sodium phosphate is an easily soluble compound that is well absorbed after parenteral administration into tissues and provides a quick effect.
Betamethasone dipropionate has a slower absorption. By combining these salts, it is possible to create medicines with both short-term (but fast) and long-term effects. Depending on the method of application (intravenous, intramuscular, intraarticular, periarticular, intravenous), a general or local effect is achieved.
Pharmacokinetics
Betamethasone sodium phosphate is highly soluble in water and, after intramuscular administration, is rapidly hydrolyzed and almost immediately absorbed from the injection site, which provides a rapid onset of therapeutic action. It is almost completely excreted within one day after administration.
Betamethasone dipropionate is slowly absorbed from the depot, metabolized gradually, which causes its long-term effect, and is excreted over more than 10 days.
Plasma protein binding of betamethasone is 62.5%. It is metabolized in the liver with the formation of predominantly inactive metabolites. It is excreted mainly by the kidneys.
Side effect
Metabolic disorders: hypernatremia, increased potassium excretion, increased calcium excretion, hypokalemic alkalosis, fluid retention in tissues, negative nitrogen balance (due to protein catabolism), lipomatosis (including mediastinal and epidural lipomatosis, which can cause neurological complications), weight gain.
From the side of the cardiovascular system: chronic heart failure (in predisposed patients), increased blood pressure.
From the musculoskeletal system: muscle weakness, steroid myopathy, loss of muscle mass, increased myasthenic symptoms in severe pseudoparalytic myasthenia gravis, osteoporosis, compression fracture of the spine, aseptic necrosis of the femoral head or humerus, pathological fractures of tubular bones, tendon ruptures, with repeated intra-articular injections).
From the digestive system: erosive and ulcerative lesions of the gastrointestinal tract with possible subsequent perforation and bleeding, pancreatitis, flatulence, hiccups.
Dermatological reactions: impaired wound healing, atrophy and thinning of the skin, petechiae, ecchymosis, excessive sweating, dermatitis, steroid acne, striae, a tendency to develop pyoderma and candidiasis, decreased reaction during skin tests.
From the nervous system: convulsions, increased intracranial pressure with edema of the optic nerve head (more often at the end of therapy), dizziness, headache, euphoria, mood changes, depression (with severe psychotic reactions), personality disorders, irritability, insomnia.
From the endocrine system: menstrual irregularities, secondary adrenal insufficiency (especially during stressful periods of illness, injury, surgery), Itsenko-Cushing's syndrome, decreased carbohydrate tolerance, steroid diabetes mellitus or manifestation of latent diabetes mellitus, increased need for insulin or oral hypoglycemic drugs, impaired intrauterine growth, growth retardation and sexual development in children.
From the side of the organ of vision: posterior subcapsular cataract, increased intraocular pressure, glaucoma, exophthalmos; in rare cases - blindness (with the introduction of the drug in the face and head).
Allergic reactions: anaphylactic reactions, shock, angioedema, arterial hypotension.
Local reactions: rarely - hyper- or hypopigmentation, subcutaneous and cutaneous atrophy, aseptic abscesses.
Others: flushing of the face after injection (or intra-articular injection), neurogenic arthropathy.
The frequency of development and the severity of side effects, as with the use of other GCS, depend on the size of the dose used and the duration of the drug. These effects are usually reversible and can be eliminated or reduced with dose reduction.
Application during pregnancy and lactation
Use during pregnancy is not recommended.
Betamethasone crosses the placental barrier. In animal studies, malformations and violations (delay) of fetal development were recorded against the background of the use of GCS during pregnancy.
With prolonged or repeated use of GCS during pregnancy, the risk of intrauterine growth retardation may increase. With the use of betamethasone during pregnancy, cases of myocardial hypertrophy and gastroesophageal reflux have been reported in newborns.
Newborns whose mothers received therapeutic doses of GCS during pregnancy should be under medical supervision (for early detection of signs of adrenal insufficiency).
Use during lactation (breastfeeding) is contraindicated.
special instructions
?анное лекарственное средство следует примен¤ть в наименьшей эффектовной дозе в течение минимального времени. Ќачальную дозу подбирают до тех пор, пока не будет достигнут необходимый терапевтический эффект. «атем постепенно снижают дозу до минимальной эффективной поддерживающей дозы. ѕри отсутствии эффекта от проводимой терапии или при его длительном применении отмена проводитс¤ постепенно, снижа¤ дозу. Ќаблюдение за состо¤нием пациента осуществл¤ют по крайней мере в течение одного года по окончании длительной терапии или применени¤ в высоких дозах.
ѕри возникновении или угрозе возникновени¤ стрессовой ситуации (не св¤занной с заболеванием) может возникнуть необходимость в увеличении дозы.
¬ведение препарата в м¤гкие ткани, в очаг поражени¤ и внутрисуставно может при выраженном местном действии одновременно привести к системному действию.
ѕри применении у пациентов с сахарным диабетом может потребоватьс¤ коррекци¤ гипогликемической терапии.
ѕациентов, получающих v —, не следует вакцинировать против оспы. Ќе следует проводить и другую иммунизацию у больных, получающих v — (особенно в высоких дозах!, ввиду возможности развити¤ неврологических осложнений и низкой ответной иммунной реакции ('отсутствие образовани¤ антител'). ќднако проведение иммунизации возможно при проведении заместительной терапии (например, при первичной недостаточности коры надпочечников).
ѕациентов, получающих данную комбинацию в дозах, подавл¤ющих иммунитет, следует предупредить о необходимости избегать контакта с больными ветр¤ной оспой и корью (особенно важно при применении препарата у детей).
¬озможно подавление реакции при проведении кожных проб на фоне применени¤ v —. —ледует учитывать, что v — способны маскировать признаки инфекционного заболевани¤, а также снижать сопротивл¤емость организма инфекци¤м
¬озможно подавление реакции при проведении кожных проб на фоне применени¤ v —.
?ействие v — усиливаетс¤ у пациентов с гипотиреозом и циррозом печени.
Ќеобходимо соблюдать осторожность при применении v — у пациентов пожилого возраста ; у пациентов с почечной или печеночной недостаточностью, дивертикулитом, активной или латентной ¤звенной болезнью желудка и/или кишечника или с наличием недавно созданных кишечных анастомозов, остеопорозом, миастенией, подтвержденными или подозреваемыми паразитарными инфекци¤ми (например, стронгилоидозом).
–азвитие вторичной недостаточности коры надпочечников в св¤зи со слишком быстрой отменой v — возможно в течение нескольких мес¤цев после окончани¤ терапии.
Ќа фоне применени¤ v — возможно изменение подвижности и числа сперматозоидов. ѕри длительной терапии v — целесообразно рассмотреть возможность перехода с парентерального на пероральное применение v —, с учетом оценки соотношени¤ польза/риск.
ѕрименение в педиатрии
?ети, которым проводитс¤ терапи¤ (особенно длительна¤) препаратом, содержащим данную комбинацию, должны находитьс¤ под тщательным медицинским наблюдением на предмет возможного отставани¤ в росте и развити¤ вторичной недостаточности коры надпочечников.
ѕрименение у спортсменов
ѕациентам, участвующим в соревновани¤х под контролем ¬семирного антидопингового агентства (WADA), перед началом лечени¤ препаратом, содержащим данную комбинацию, следует ознакомитьс¤ с правилами WADA, поскольку применение таких препаратов может повли¤ть на результаты допингового контрол¤.
Ћекарственное взаимодействие
ѕри одновременном применении фенобарбитала, рифампицина, фенитоина или эфедрина возможно ускорение метаболизма бетаметазона при снижении его терапевтической активности.
ѕри одновременном применении v — и эстрогенов может потребоватьс¤ коррекци¤ дозы бетаметазона (из-за риска передозировки).
ѕри совместном применении бетаметазона и калийвывод¤щих диуретиков повышаетс¤ веро¤тность развити¤ гипокалиемии.
ќдновременное применение v — и сердечных гликозидов повышает риск возникновени¤ аритмии или дигиталисной интоксикации (из-за гипокалиемии). Ѕетаметазон может усиливать выведение кали¤, вызванное амфотерицином ¬.
ѕри совместном применении бетаметазона и непр¤мых антикоагул¤нтов возможны изменени¤ свертываемости крови, требующие коррекции дозы антикоагул¤нтов.
ѕри комбинированном применении v — с Ќѕ¬— или с этанолом и этанолсодержащими препаратами возможно повышение частоты развити¤ или интенсивности эрозивно-¤звенных поражений ? “.
ѕри совместном применении v — могут снизить концентрацию салицилатов в плазме крови.
ќдновременное введение v — и соматотропина может привести к замедлению абсорбции последнего (следует избегать введени¤ доз бетаметазона, превышающих 300-450 мкг/м2/сут).
v — могут вли¤ть на азотный голубой тетразолевый тест на бактериальную инфекцию и вызывать ложно-отрицательный результат.
јминоглутетимид может вызвать снижение вызванного кортикостероидами подавлени¤ функции надпочечников.
ѕри одновременном применении v — и кетоконазола или итраконазола возможно усиление системных побочных эффектов v —.
v — способны уменьшать эффект ингибиторов холинэстеразы, что может привести к развитию выраженной мышечной слабости у пациентов с миастенией. ѕо возможности, ингибиторы холинэстеразы должны быть отменены, по крайней мере, за 24 ч до начала терапии v —.
ѕри одновременном применении v — и изониазида возможно снижение концентрации изониазида в плазме крови. —ледует тщательно контролировать состо¤ние пациентов, принимающих изониазид.
The simultaneous use of cyclosporine and corticosteroids can lead to an increase in the concentration of ciclosporin and an increase in the action of corticosteroids. There is a high risk of developing seizures.
With the simultaneous use of GCS with antibiotics of the macrolide group, a significant decrease in the excretion of GCS is possible.
With simultaneous use with cholestyramine, it is possible to increase the excretion of corticosteroids.